Background:
Tramadol (TR) is an opioid agonist (μ-opioid receptors) that also affects the noradrenergic and serotonergic systems. TR is a synthetic analgesic substance with opioid agonist properties that has been approved for pain management by affecting the central nervous system.
Objective:
The primary objective of this scoping review was to determine the poisoning consequences of TR and its associated symptom management techniques, as well as its effect on opioid and non-opioid receptors, metabolism, and complications on various organ systems.
Discussion:
Typically, acute overdose of TR is not considered life threatening, and most fatalities are attributed to polysubstance overdose. TR can cause drowsiness, headaches, seizures, respiratory depression, low heart rate, coma, and even death. Additionally, the prolonged use of TR can lead to addiction, with withdrawal resulting in both common and atypical symptoms.
Conclusions:
Therefore, it is recommended that patients with TR poisoning receive close monitoring of their cardiovascular system, along with a comprehensive management plan for their levels of consciousness and respiratory function.
Keywords: complications, opioid, poisoning, tramadol
Introduction
Highlights
Tramadol (TR) is a synthetic analgesic drug with opioid agonist properties.
TR can cause drowsiness, headaches, seizures, and respiratory depression.
Acute TR overdose is generally not life threatening, and the majority of fatalities are due to polysubstance overdose.
Tramadol (TR), also known as Ultram, is a type of opioid agonist that targets the μ-opioid receptors (μ-ORs), as well as the noradrenergic and serotonergic systems. It was initially synthesized in 1962 and has been utilized as a pharmaceutical analgesic since 19771. TR, a synthetic analgesic drug, has been approved by the Food and Drug Administration (FDA) since 1995 for the management of pain. It exerts its effect by acting as an opioid agonist and affects the central nervous system (CNS). This drug is available to patients in various forms, including drops, intravenous (IV) solutions, subcutaneous (SQ), and extended-release preparations2–5.
After oral administration, TR is rapidly absorbed into the bloodstream, but its bioavailability is ~70% due to hepatic metabolism. Despite this, the drug is able to cross the blood–brain barrier and exert its opioid agonist effects centrally. Interestingly, buccal and nasal administration routes can result in much higher bioavailability, with nasal administration resulting in ~500% and buccal administration resulting in around 200% bioavailability when compared to oral administration6.
TR, a racemic combination containing two enantiomers, acts synergistically as both the positive enantiomers (+) and negative enantiomers (−) have distinct pharmacological effects, with the (+) enantiomers binding with μ and κ-opioid receptors as well as inhibiting norepinephrine (NE) and 5-HT reuptake, while the (−) enantiomers only inhibit NE reuptake7–9. Compared to morphine (which has an affinity 6000 times greater) and codeine (10 times greater), TR demonstrates significantly lower binding affinity for μ-ORs10. The potent chemical actions of TR’s primary metabolite, O-desmethyltramadol, which are facilitated by CYP2D6, include significant inhibition of both NE and 5-HT reuptake, as well as agonistic interaction with the μ-ORs, exhibiting an agonist effect that is 200-fold more potent than TR itself11.
For cancer patients, as well as those experiencing conditions such as spinal cord injury, low back pain, rheumatoid arthritis, and various types of acute pain (including abdominal and labor pain), this opioid analgesic is frequently administered, either alone or in combination with other non-steroidal anti-inflammatory drugs (NSAIDs)12,13. TR has demonstrated efficacy in the treatment of neuropathic pain14, fibromyalgia, and osteoarthritis-related pain15. In addition to its use in pain management, there is some evidence that TR is utilized in the treatment of premature ejaculation16,17.
The recommended doses for TR include 50 mg orally, 50–100 mg injectable, and 100 mg rectally, with a daily maximum of 400 mg, while therapeutic blood levels for adults range from 100 to 300 ng/ml (0.1–0.3 µg/ml) and for children, doses range from 1 to 2 mg/kg/dose; the lethal dose of TR has not been established, and in combination with other drugs, its fatal level is extremely low (0.15–39 mg/l)18.
Acute TR overdose is generally non-life-threatening, and the majority of fatalities are attributed to polysubstance overdose. An acute overdose of TR can result in symptoms such as miosis, tachycardia, seizures, CNS suppression, coma, respiratory depression, hypotonicity, and acidosis19. On the other hand, chronic TR use or abuse may cause several adverse effects that include fatigue, dizziness, vertigo, headache, visual disturbances, nausea, vomiting, sweating, dry mouth, constipation, postural hypotension, irregular heartbeats, euphoria, dysphoria, and hallucinations20. According to reliable sources, acute kidney injury (AKI) is not a common consequence of TR poisoning, and information regarding its prevalence and treatment is limited, but there have been cases of AKI following TR toxicity in recent years21–23.
TR is similar to other opioids in that long-term use can develop opioid physical dependency, which can be followed by a withdrawal syndrome if the drug is suddenly discontinued24,25. In contrast to numerous other opioids, TR has an effect on numerous neurotransmitter systems, such as the opioid system and the serotonin and NE systems, among others. The opioid antagonist, naloxone, only partly inhibits the actions of TR26,27, and there is minimal cross-tolerance with other opioids25,28–30, suggesting that the cumulative influence of the drug is due to its effects on multiple systems. The aim of this scoping review was to determine the consequences of TR poisoning, including the best methods of managing associated symptoms, as well as examining its metabolism and effects on both opioid and non-opioid receptors (ORs), and the complications that may arise in multiple organ systems (see Table 1). This analysis was reviewed and approved by the Mazandaran University of Medical Science Ethics Committee (No.: IR.MAZUMS.REC.1399.7850) and was carried out in accordance with the Helsinki Declaration Principles. This study is registered with the Research Registry, and the UIN is research registry 8622 (https://www.researchregistry.com/register-now#home/registrationdetails/63c521df4817670011b960fa/).
Table 1.
Pharmacokinetic, pharmacodynamic, and clinical complications of tramadol
| Parameter | Descriptions | |
|---|---|---|
| Absorption | Oral, SQ, injectable | |
| Excretion | Kidney | |
| Mechanism of action | μ-ORs, NE, and serotonin inhibition | |
| Therapeutic dose | 0.1–0.3 mg/l (adults); 1–2 mg/kg/dose (children) | |
| Lethal dose | 0.15–39 mg/l | |
| Pregnancy time | Category C | |
| Drug interaction | Antidepressants, digoxin, rifampin carbamazepine, MAOIs, quinidine | |
| Antidote | BZDs, naloxone | |
| Complications | Pupil | Miosis, mydriasis |
| Brain | Seizures | |
| Heart | Dysrhythmia | |
| Lung | Apnea | |
| Neurology | Serotonin syndrome | |
| Kidney | Renal failure | |
| Shoulder | Dislocation | |
| Muscle | Rhabdomyolysis | |
BZDs, benzodiazepines; MAOIs, monoamine oxidase inhibitors; NE, norepinephrine; μ-ORs, μ-opioid receptors; SQ, subcutaneous.
Discussion
Pharmacokinetics and pharmacodynamics
TR can be administered via oral, IV, or SQ routes of administration31. Novel transdermal routes have been developed to address the limitations of the conventional therapeutic methods32. When administered orally, TR is administered in its racemic form, achieving swift and comprehensive absorption in the intestine, allowing for a bioavailability of 70%33. TR undergoes extensive metabolism following absorption, which includes O-demethylation and N-demethylation, conjugation, and urine excretion. The elimination half-life (β elimination) of the drug is ~5 h, while that of its main metabolite is around 8 h. TR is mostly eliminated by the kidneys (~90%), with the remainder passing through the feces. Patients with renal failure exhibit diminished TR excretion in comparison to healthy individuals34. Notably, the concentration of TR in the urine is one order of magnitude higher than that of cardiac blood, peripheral blood, liver, and kidney tissue35.
The elimination of TR is primarily attributed to renal clearance, accounting for over 90% of its elimination, with minimal activity detected in fecal or salivary specimens. Moreover, following the intramuscular administration of TR (50 mg), a significant increase in the concentration of the drug within both urine and saliva samples was observed after just 30 min36.
Mechanism of action
The mechanism of action of TR is primarily through the activation of ORs, which is well-established and understood. Specifically, TR binds to μ-ORs with moderate affinity and 6 and κ ORs with weak affinity, although the affinity is considerably lower compared to codeine and morphine. In addition to ORs, TR demonstrates activity with monoamine transporters, such as NE and serotonin, through the inhibition of monoamine reuptake, subsequently diminishing the transmission of pain signals within the CNS37.
Drug interaction
The morbidity and mortality rates associated with TR poisoning are primarily attributed to drug interactions. Specifically, over 761 substances have been identified to interact with this drug. Antidepressants, carbamazepine, digoxin, monoamine oxidase (MAO) inhibitors, rifampin, quinidine, stress medications, sedatives, alcohol, and blood thinners have been identified as some of the frequently prescribed medications that contribute to TR poisoning38. Serotonin syndrome (SS) is caused by the combination of TR and serotonin inhibitors like fluoxetine. TR inhibited serotonin reuptake, resulting in a rise in plasma serotonin levels and serotonin release at high dosages39,40. Furthermore, the main signs of SS, mydriasis and tachycardia, have been identified as significant risk factors for seizure41,42.
TR in pregnancy and lactation
TR and its active metabolite, O-desmethyltramadol, have demonstrated a propensity for crossing the placenta. An experimental study was conducted on women undergoing labor analgesia with intramuscular doses of TR, reaching a maximum of 250 mg. Results of this study revealed that the mean concentration of TR in the fetus at delivery was found to be 94 (±13)%43. Due to the lack of human evidence in pregnancy, the product information leaflet advises that TR should not be used in pregnant women before or during labor, unless the potential benefits outweigh the risks44. Unfortunately, no major case–control or cohort studies of pregnant women who were exposed to TR throughout their pregnancy exist.
The Australian Therapeutic Goods Administration Evaluation Committee (ATGAEC) has classified TR as a category C drug45. This classification denotes substances that are capable of inducing detrimental effects on the human fetus or neonate, attributable to their pharmacological effects, with potential for reversibility but without causing abnormalities. Based on the available evidence, it is recommended to abstain from using TR both at the time of conception and during organogenesis, as this appears to be the safest course of action. While TR is not approved for use in breastfeeding mothers, it has been administered to provide pain relief for women who have undergone a cesarean section or have perineal injuries. Typically, for drugs that do not manifest appreciable toxicity to an infant, a relative infant dosage of less than 10% is deemed acceptable to prevent any potential harm to a full-term newborn46.
TR dependency
TR dependency is associated with dopamine release in several areas of the CNS. Agonists of μ-ORs enhance dopamine release while reducing the release of γ-aminobutyric acid, which inhibits dopamine release47. The use of TR has been linked to a heightened risk of dependency, as both TR itself and its metabolites function as agonists at μ-ORs. Despite initial assumptions of a relatively low risk for dependency, the widespread use of TR for prolonged pain management and its misuse in the context of drug abuse has led to the recognition of a substantial dependency rate48.
TR has been used as an analgesic in Iran for numerous years, and its sale and distribution are unrestricted. TR abuse, on the other hand, is on the increase due to the high number of drug users. Some drug users use it to quit using opiates without a prescription, which increases the incidence of addiction. As a result, more addicts are developing TR dependency, which is followed by withdrawal symptoms. When compared to other opioids, TR dependency is quite uncommon. Following its original introduction, an independent steering committee in the United States was established to monitor TR abuse and dependency. They found a frequency of dependence of less than 1 in 100 000 patients49.
Withdrawal of TR
TR withdrawal symptoms can be classified as either typical or atypical. So far, only a few unusual symptoms associated with TR withdrawal have been described. The most common symptoms of TR withdrawal include musculoskeletal and gastrointestinal pain, anxiety, depression, diarrhea, insomnia, lacrimation, nausea, agitation, rhinorrhea, and excessive sweating. Unusual CNS symptoms such as confusion, delusion, derealization, depersonalization, and paranoid thoughts (2.27% prevalence), unnatural sensory experiences such as numbness, tingling, prickling, and tinnitus (4.25% prevalence), and tactile, visual, and auditory hallucinations are all examples of atypical symptoms (20% prevalence)50. The combination of clonidine (for the treatment of diarrhea, lacrimation, rhinorrhea, and nausea), baclofen, and ibuprofen (NSAID) is particularly beneficial in the decrease and termination of TR withdrawal and craving for severe TR withdrawal.
Withdrawal syndrome in the neonate
TR use during pregnancy is classified as a category C drug, which induces serotonin release whilst inhibiting NE reuptake. Prolonged use of this substance during pregnancy, whether due to low back discomfort, headaches, or other addictive tendencies, may lead to physical dependency and subsequent withdrawal symptoms in the newborn infant. Nausea, vomiting, poor feeding, agitation, tremors, hypertonicity, multifocal myoclonus, tachycardia, tachypnea, and generalized tonic–clonic seizures can all be indications of withdrawal syndrome 24 h after delivery51. The optimal drug for managing neonatal TR withdrawal is unknown. The withdrawal syndrome may be caused by both opioid and non-opioid actions (particularly the suppression of 5-HT reuptake). Benzodiazepines (BZDs), phenobarbital, clonidine, and opium tincture have all been recommended as treatments52.
Clinical complications
The clinical manifestations of TR poisoning can comprise a range of serious consequences, such as seizures, rhabdomyolysis, renal failure, shoulder dislocation, respiratory depression, SS, cardiac events, and, in some instances, even death (see Fig. 1). The incidence of TR poisoning and fatalities has been observed to be mounting, and reports concerning the abuse and resulting toxicity of this substance are likewise increasing53. Long-term use of TR has been associated with numerous adverse effects, including vertigo, hyperglycemia, hypotonicity, seizures, SS, headache, acidosis, ear infection, tinnitus, and vertigo in rare cases39,54–56.
Figure 1.
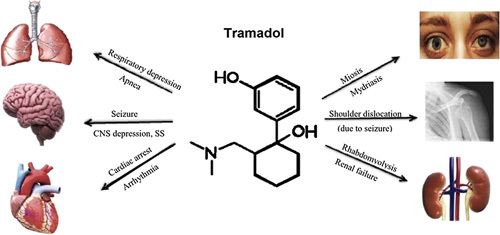
Clinical complications of tramadol on various organs.
Seizures
Seizures are a common side effect of TR usage, although the specific mechanism of TR-induced seizures is unknown. The most frequent adverse neurological symptoms documented in TR-intoxicated individuals are seizures and loss of consciousness. These can occur at both therapeutic and toxic dosages. Although BZDs can manage TR-related seizures, several studies have shown that BZDs, even at therapeutic doses, may enhance the morbidity and mortality of TR overdoses57.
TR’s anti-nociceptive effects appear to be associated with its inhibition of serotonin absorption and agonism at the μ and κ ORs. The serotonergic effect appears to be mediated by the 5HT2 receptor. TR’s abuse potential is most probably due to antagonism at the opioid κ receptor. In this regard, TR is comparable to the κ receptor agonist salvinorin A, the main hallucinogenic element in the frequently abused Salvia divinorum plant58.
TR-induced seizures usually happen during the first 4–6 h after consuming too much TR. These seizures are generally single, brief, generalized tonic–clonic episodes that last less than 5 min. In population-based research, the prevalence of TR-related seizures ranges from 0.15 to 0.86%. TR dosages that cause seizures vary from 100 to 500 mg. Although it does not appear to be dose dependent, higher TR doses increase the risk. According to new evidence, the majority of seizures occur in younger individuals who abuse TR at dosages greater than 1000 mg. The risk of seizures appears to be higher when combined with serotonergic psychotropic cytochrome P-450 2D6 inhibitors, which lower the seizure threshold even further. Younger individuals are more likely to abuse drugs, and they are more likely to overdose on greater dosages of TR. Adults between the ages of 25 and 44 were found to be most at risk for seizures, with a mean age of 25 years.
The physical injury to the head is the most common adverse effect of seizures, which affects up to 1% of patients. Administration of a BZD such as lorazepam, supportive therapy to minimize damage, and discontinuation of TR and other proconvulsant serotonergic drugs are all options for treatment59.
Serotonin syndrome
The occurrence of SS subsequent to TR usage is atypical.TR rarely causes SS, which manifests as hallucinations, tachycardia, hyperthermia, hyperreflexia, and coma due to TR’s effect on serotonin reuptake inhibition. TR should not be used with serotonin reuptake inhibitors (SSRIs), selective NE reuptake inhibitors (SNRIs), triptans, MAO inhibitors, or tricyclic antidepressants since they have comparable serotonergic effects.
SS manifests through a cluster of symptoms that vary in their degrees of severity. Neuromuscular hyperactivity, autonomic hyperactivity, and altered mental state make up the traditional triad. Mild types contain nonspecific symptoms, including sweating, tremors, and enhanced reflexes, and are commonly misdiagnosed and untreated. Rhabdomyolysis, myoglobinuria, renal failure, disseminated intravascular coagulation (DIC), metabolic acidosis, and acute respiratory distress syndrome (ARDS) are all complications of SS60.
SS has been described in concomitant use with serotonergic psychotropic drugs such as fluoxetine, paroxetine, sertraline, venlafaxine, mirtazapine, citalopram, bupropion, olanzapine, clozapine, ziprasidone, and razagilin. Certain serotonergic antidepressants (e.g. paroxetine, fluoxetine) that inhibit cytochrome P-450 2D6 by raising TR blood levels also increase the risk of SS61.
SS induced by TR is a medical emergency that poses a threat to life and requires urgent treatment in an emergency department.TR and other serotonergic drugs are discontinued, and intensive supportive care is performed to manage agitation, hyperthermia, and autonomic dysfunction. IV fluids, cardiac monitoring, cooling blankets, and oxygen therapy to maintain saturations greater than or equal to 94% are all life-saving interventions. For agitation, antipsychotics and restraints are preferable over BZDs. Antipyretics are not recommended for hyperthermia because the higher temperature is caused by increased muscular activity rather than a change in the hypothalamus thermal set point. Administering cyproheptadine, an antidote for SS, is advisable for patients with moderate to severe symptoms or those who do not respond to supportive therapy alone. Initially, 12 mg of cyproheptadine should be given, followed by 2 mg every 2 h until the symptoms improve. The daily cyproheptadine dosage varies based on individual situations, but studies indicate that taking 12–18 mg of cyproheptadine blocks 85–95% of 5HT2 receptors62.
Rhabdomyolysis and renal failure
Rhabdomyolysis is the release of muscle cell contents into the bloodstream as a consequence of skeletal muscle trauma. It can result from severe muscular damage, such as that caused by a crushing injury or an electrical shock. Cocaine, heroin, ethanol, amphetamines, and caffeine are examples of drugs or poisons that can cause this disorder. TR is a relatively uncommon cause of rhabdomyolysis and renal failure, with just a few cases described in the literature.
Due to the wide range of causes, the clinical presentation of rhabdomyolysis is extremely variable. Acute myalgia and pigmenturia due to myoglobinuria, as well as increased serum creatine phosphokinase, are the hallmark symptoms of rhabdomyolysis. Compartment syndrome, hyperkalemia, hypocalcemia, elevated liver enzymes, cardiac arrhythmias, acute renal failure (ARF), and DIC can also be mentioned. Rhabdomyolysis is treated with prompt and aggressive fluid resuscitation, the elimination of causative factors, and the treatment and prevention of any complications that may occur. Supportive therapy, including hydration and alkalinization of urine with sodium bicarbonate, is essential in patients with rhabdomyolysis and appropriate urinary output. If there is no response to treatment, dialysis is recommended21.
Shoulder dislocation
The administration of TR, within therapeutic or toxic levels, can trigger seizures, typically characterized as a generalized tonic–clonic seizure, observed within the initial 24 h post-consumption. Young individuals with prolonged history of drug ingestion, and those who consume alcohol concomitantly, are more susceptible to experiencing these seizures63. However, seizures are uncommon at therapeutic doses, with a prevalence of less than 1% described. In epileptic patients, a seizure can cause a posterior shoulder dislocation. Axial loading in adduction and internal rotation of the arm due to severe muscle contraction during seizure is the cause of injury64.
Anterior shoulder dislocation is a frequently reported issue in the emergency medicine domain. Following a comprehensive physical examination and confirming the results by utilizing the appropriate X-ray, the majority of emergency physicians are capable of rendering a prompt diagnosis for anterior shoulder dislocation65. As compared to anterior dislocation, posterior dislocation of the shoulder is an uncommon occurrence that is sometimes missed on initial inspection. Clinical manifestations are occasionally minimal or nonexistent, and X-rays may be inconclusive, making diagnosis challenging.
Respiratory depression
Despite the minimal potential for adverse effects from TR, there have been documented cases of addiction and respiratory depression. Respiratory depression triggered by TR is rare, with increased frequency in individuals that exhibit CYP2D6 duplication (high metabolizers). Given the considerable variability in CYP2D6 expression across individuals, the analgesic effect of TR exhibits wide-ranging differences among patients21. Unlike several other opioids, there have been relatively few reports of TR-induced respiratory depression and apnea published in scientific literature. However, renal insufficiency has been identified as a potential risk factor. IV administration of TR, which can induce apnea and result in a fatality, has been reported to have a non-respiratory cause66. Apnea induced by TR ingestion may manifest up to 24 h following consumption and is not typically associated with CNS depression or seizures. In clinical trials involving oral administration of TR, fatalities were attributed to the concurrent use of multiple CNS depressants, including barbiturates, BZDs, and/or medications featuring serotonergic properties67. The oral dose of 100 mg TR suppressed respiration in ten healthy individuals by reducing ventilatory CO2 sensitivity by 30% without changing metabolic or arousal states. In healthy volunteers without pain, the effect of 100 mg TR is shown to be similar to that of 0.13 mg/kg IV morphine68. Therefore, individuals receiving therapeutic dosages of TR may have severe opioid symptoms.
Presently, there is a lack of clinical research assessing the prevalence of apnea among individuals who have exclusively utilized oral TR. Furthermore, while Spiller et al.69 identified respiratory depression in 2 (2%) out of 87 individuals who used TR alone, the route of use was not specified. There seems to be a significant correlation between the dosage of TR and the incidence of respiratory depression70.
Cardiovascular events
TR causes mild hypertension and tachycardia by increasing the concentration of NE in the brain. Complications of long-term use of TR include dizziness, headaches, dry mouth, premature heartbeat, hallucinations, and visual disturbances71. Ingesting 5 g of TR has been associated with a rare side effect of cardiopulmonary arrest72. Similar to other drug toxicities, cardiac symptoms may also manifest in TR poisoning. The most frequently observed symptoms are usually mild electrocardiographic (ECG) alterations such as sinus tachycardia, though more severe conditions may also occur. Research suggests that an overdose of TR can lead to sinus tachycardia, QTC prolongation, and QRS widening. These conditions can often be attributed to the drug’s inhibitory effect on fast sodium and potassium channels73.
Numerous cases of cardiovascular disorders have been reported subsequent to TR poisoning or overdose74. In these patients, ventricular arrhythmias followed by cardiac arrest with refractory cardiogenic shock usually occur. Furthermore, IV TR administration has been related to Kounis syndrome, an allergic reaction characterized by clinical features and findings of acute coronary syndrome stimulated by inflammatory cytokines and mast cell activation75 in patients who were previously healthy and had no cardiovascular risk factors. Dyspnea, palpitations, chest discomfort, and hemodynamic instability appeared shortly after infusion, prompting a diagnosis of myocardial infarction (MI)76. Previous studies on drugs with similar pharmacologic properties may provide some insight into TR’s potential cardiovascular effects. Antidepressants such as SSRIs have a mechanism similar to TR, and the existing research on SSRIs and the risk of MI is conflicting. Prolonged QT intervals can lead to the onset of arrhythmias or serious instances of torsade de pointes, both of which can result in sudden cardiac death77.
Fatal dose
Typically, the therapeutic range for TR is between 0.1 and 0.3 mg/l. Fatalities caused by TR poisoning are rare. The precise lethal dose of TR remains unknown. However, if TR is concurrently ingested with other medications, it has been noted that the lethal dose for such cases can be notably low, ranging from 0.15 to 39 mg/l18. TR overdose fatalities have been reported to occur with a blood concentration of 15.1 mg/l. It is possible that the underlying pathophysiological mechanism of TR overdose is respiratory depression. Our study’s results indicate that even in the absence of interacting medications, large doses of TR can cause mortality. This finding is consistent with prior research78.
Management and antidote
TR overdose or intoxication may be associated with a decreased level of consciousness, seizures, respiratory depression, and SS79,80. For controlling TR side effects, many medication combinations were considered. Among these, using naloxone to treat a TR-induced seizure is still controversial. However, the basis of treatment for TR poisoning involves cardiovascular monitoring as well as the insertion of a nasogastric tube (NGT), administration of charcoal and sorbitol, hydration, control of seizures with BZDs, and treatment of respiratory depression with naloxone. Additionally, various studies have reported on the efficacy of using intralipid emulsion (ILE) as an adjunct to standard antidote protocols for treating hemodynamic symptoms or seizures resulting from poisoning with lipophilic compounds, such as TR. ILE has been found to be effective by increasing left ventricular contractility81.
Conclusion
TR is widely used in the reduction of acute and chronic pain, especially toothaches and cancer pain, as well as the management of labor pains. Because TR can induce its effects through different receptors, it is possible that TR may interact with other drugs, particularly medications with the same metabolism. So, to prevent the unpredictable side effects of TR, careful monitoring of its drug interactions is essential. TR overdose has been identified as one of the most frequent causes of drug poisoning in young male adults with a history of mental illness and substance abuse. Symptoms commonly observed in cases of TR overdose include tachycardia, nausea, vomiting, CNS depression, and seizures. Cardiopulmonary arrest has been identified as the most common cause of death in TR poisoning. As a result, it suggests that close monitoring of the cardiovascular system, as well as management of the patient’s level of consciousness and respiratory system, is required in patients with TR poisoning.
Key points
TR is a synthetic analgesic drug with opioid agonist (μ-opioid receptor) properties.
TR is rapidly absorbed after oral administration, with more than 90% of the drug eliminated renally.
TR is a NE and 5-HT reuptake inhibitor with an active metabolite (O-desmethyltramadol).
TR therapeutic dose in adults ranges from 100 to 300 ng/ml (0.1–0.3 µg/ml) and in children 1–2 mg/kg/dose.
TR overdose fatalities occur with a blood concentration of 15.1 mg/l.
TR and its active metabolite readily cross the placenta and are classified as category C drugs.
The most common symptoms of TR withdrawal include musculoskeletal pain, anxiety, diarrhea, agitation, rhinorrhea, and excessive sweating.
The most common neurological symptom in TR poisoning is seizures and decreased level of consciousness.
Serotonin syndrome is a rare occurrence with TR use, and its antidote is cyproheptadine.
Anterior shoulder dislocation is a frequent complaint resulting from TR-induced seizures.
Respiratory depression induced by TR is rare, and naloxone is the antidote.
Sinus tachycardia is the most common cardiac manifestation observed in cases of TR overdose.
The management of TR poisoning includes cardiovascular monitoring, activated charcoal administration, hydration, and treatment of seizures and respiratory depression.
Future perspective
Increasing public awareness about the many side effects of TR.
Restrict the use of TR to young individuals.
Production of a new generation of TR with fewer side effects.
TR is administered only to hospitalized patients to control pain and withdrawal symptoms.
Ethical approval
This research was approved by the Mazandaran University of Medical Science Ethics Committee (No: IR.MAZUMS.REC.1399.7850) and was carried out in accordance with the Helsinki Declaration Principles.
Consent
Not applicable.
Sources of funding
The study was funded by the Mazandaran University of Medical Sciences. The funder has no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author contribution
Z.N. and Z.Z.: designed the study and wrote the manuscript; A.A.M.: involved in interpretation and editing the manuscript; A.M. and Z.Z.: responsible for collecting data and submitting the manuscript. All the authors reviewed the paper and approved the final version of the manuscript.
Conflicts of interest disclosure
The authors have no conflicts of interest to declare.
Research registration unique identifying number (UIN)
Name of the registry: not applicable.
Unique identifying number or registration ID: 8622.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/register-now#home/registrationdetails/63c521df4817670011b960fa/.
Guarantor
Zahra Nekoukar.
Data availability statement
The authors are responsible for data. Access to all relevant raw data will be free to any scientist.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgements
Not applicable.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 7 July 2023
Contributor Information
Aliasghar Manouchehri, Email: Manouchehriaa@yahoo.com.
Zahra Nekoukar, Email: NekoukarZ108@yahoo.com.
Abdollah Malakian, Email: drmalakian9@gmail.com.
Zakaria Zakariaei, Email: ali.zakariaei@yahoo.com.
References
- 1.Grond S, Sablotzki A. Clinical pharmacology of tramadol. Clin Pharmacokinet 2004;43:879–923. [DOI] [PubMed] [Google Scholar]
- 2.Casella S, Giannetto C, Giudice E, et al. ADP-induced platelet aggregation after addition of tramadol in vitro in fed and fasted horse’s plasma. Res Vet Sci 2013;94:325–330. [DOI] [PubMed] [Google Scholar]
- 3.Lavasani H, Sheikholeslami B, Ardakani YH, et al. Study of the pharmacokinetic changes of Tramadol in diabetic rats. Daru 2013;21:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eassa BI, El-Shazly MA. Safety and efficacy of tramadol hydrochloride on treatment of premature ejaculation. Asian J Androl 2011;17:538–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Domínguez-Oliva A, Casas-Alvarado A, Miranda-Cortés AE, et al. Clinical pharmacology of tramadol and tapentadol, and their therapeutic efficacy in different models of acute and chronic pain in dogs and cats. J Adv Vet Anim Res 2021;8:404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang H, Zhao Y, Wang X, et al. Bioavailability of tramadol hydrochloride after administration via different routes in rats. Biopharm Drug Dispos 2014;35:525–531. [DOI] [PubMed] [Google Scholar]
- 7.Modi H, Mazumdar B, Bhatt J. Study of interaction of tramadol with amlodipine in mice. Indian J Pharmacol 2013;45:76–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Minami K, Uezono Y, Ueta Y. Pharmacological aspects of the effects of tramadol on G-protein coupled receptors. J Pharmacol Sci 2007;103:253–260. [DOI] [PubMed] [Google Scholar]
- 9.Raffa RB, Friderichs E, Reimann W, et al. Complementary and synergistic antinociceptive interaction between the enantiomers of tramadol. J Pharmacol Exp Ther 1993;267:331–340. [PubMed] [Google Scholar]
- 10.Gillen C, Haurand M, Kobelt DJ, et al. Affinity, potency and efficacy of tramadol and its metabolites at the cloned human µ-opioid receptor. Naunyn-Schmiedeberg’s Arch Pharmacol 2000;362:116–121. [DOI] [PubMed] [Google Scholar]
- 11.Hartrick CT, Rozek RJ. Tapentadol in pain management: a μ-opioid receptor agonist and noradrenaline reuptake inhibitor. CNS Drugs 2011;25:359–370. [DOI] [PubMed] [Google Scholar]
- 12.Tetsunaga T, Tetsunaga T, Tanaka M, et al. Efficacy of tramadol–acetaminophen tablets in low back pain patients with depression. J Orthop Sci 2015;20:281–286. [DOI] [PubMed] [Google Scholar]
- 13.Kostev K, Von Vultée C, Usinger DM, et al. Tramadol prescription patterns in patients followed by general practitioners and orthopedists in Germany in the year 2015. Postgrad Med 2018;130:37–41. [DOI] [PubMed] [Google Scholar]
- 14.Hollingshead J, Dühmke RM, Cornblath DR. Tramadol for neuropathic pain. Cochrane Database Syst Rev 2006;19:CD003726. [DOI] [PubMed] [Google Scholar]
- 15.Fernandes L, Hagen KB, Bijlsma JW, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Annals of the rheumatic diseases 2013;72:1125–35. [DOI] [PubMed] [Google Scholar]
- 16.Martyn-St James M, Cooper K, Kaltenthaler E, et al. Tramadol for premature ejaculation: a systematic review and meta-analysis sexual function and fertility. BMC Urol 2015;30:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirby EW, Carson CC, Coward RM. Tramadol for the management of premature ejaculation: a timely systematic review. Int J Impot Res 2015;27:121–127. [DOI] [PubMed] [Google Scholar]
- 18.Nakhaee S, Mehrpour O. Tramadol poisoning-associated mortality. J Affect Disord 2019;1:165–0327.. [DOI] [PubMed] [Google Scholar]
- 19.Mike TB, DeVault H, Blackford MG. Acute tramadol ingestion with transient acute kidney injury in an adolescent female. J Pediatr Pharmacol Ther 2021;26:411–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mood NE, Sabzghabaee AM, Safdari A, et al. Clinical signs, hospitalization duration and outcome of tramadol intoxication. J Isfahan Med Sch 2011;28:1187–1193. [Google Scholar]
- 21.Gholami F, Sadeghi M, Zakariaei Z, et al. Rhabdomyolysis and acute kidney injury due to suicide attempt with tramadol: a rare case report. Clin Case Rep 2022;10:e05255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang SQ, Li CS, Song YG. Multiply organ dysfunction syndrome due to tramadol intoxication alone. Am J Emerg Med 2009;27:903.e57. [DOI] [PubMed] [Google Scholar]
- 23.Dogar SA, Khan FA. Tramadol-paracetamol combination for postoperative pain relief in elective single-level microdisectomy surgery. J Neurosurg Anesthesiol 2017;29:157–160. [DOI] [PubMed] [Google Scholar]
- 24.Carroll CP, Walsh SL, Bigelow GE, et al. Assessment of agonist and antagonist effects of tramadol in opioid-dependent humans. Exp Clinical Psychopharmacol 2006;14:109. [DOI] [PubMed] [Google Scholar]
- 25.Lofwall MR, Walsh SL, Bigelow GE, et al. Modest opioid withdrawal suppression efficacy of oral tramadol in humans. Psychopharmacology 2007;194:381–393. [DOI] [PubMed] [Google Scholar]
- 26.Apaydin S, Uyar M, Karabay NU, et al. The antinociceptive effect of tramadol on a model of neuropathic pain in rats. Life Sci 2000;66:1627–1637. [DOI] [PubMed] [Google Scholar]
- 27.Desmeules JA, Piguet V, Collart L, et al. Contribution of monoaminergic modulation to the analgesic effect of tramadol. Br J Clin Pharmacol 1996;41:7–12. [DOI] [PubMed] [Google Scholar]
- 28.Dunn KE, Tompkins DA, Bigelow GE, et al. Efficacy of tramadol extended-release for opioid withdrawal: a randomized clinical trial. JAMA Psychiatry 2017;9:885–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lanier RK, Lofwall MR, Mintzer MZ, et al. Physical dependence potential of daily tramadol dosing in humans. Psychopharmacology 2010;211:457–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lofwall MR, Babalonis S, Nuzzo PA, et al. Efficacy of extended-release tramadol for treatment of prescription opioid withdrawal: a two-phase randomized controlled trial. Drug Alcohol Depend 2013;133:188–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ray J, Jordan D, Pinelli C, et al. Case studies of compounded tramadol use in cats. Int J Pharm Compd 2012;16:44–49. [PubMed] [Google Scholar]
- 32.Lamont LA. Adjunctive analgesic therapy in veterinary medicine. Veterinary Clinics of North America: Small Animal Practice. 2008;38:1187–203. [DOI] [PubMed] [Google Scholar]
- 33.Lintz W, Becker R, Gerloff J, et al. Pharmacokinetics of tramadol and bioavailability of enteral tramadol formulations. 4th Communication: drops (without ethanol). Arzneimittel-forschung 2000;50:99–108. [DOI] [PubMed] [Google Scholar]
- 34.Paar WD, Frankus P, Dengler HJ. The metabolism of tramadol by human liver microsomes. Clin Investig 1992;70:708–710. [DOI] [PubMed] [Google Scholar]
- 35.Levine B, Ramcharitar V, Smialek JE. Tramadol distribution in four postmortem cases. Forensic Sci Int 1997;86:43–48. [DOI] [PubMed] [Google Scholar]
- 36.Lintz W, Beier H, Gerloff J. Bioavailability of tramadol after i.m. injection in comparison to i.v. infusion. Int J Clin Pharmacol Ther 1999;37:175–183. [PubMed] [Google Scholar]
- 37.Reimann W, Hennies HH. Inhibition of spinal noradrenaline uptake in rats by the centrally acting analgesic tramadol. Biochem Pharmacol 1994;47:2289–2293. [DOI] [PubMed] [Google Scholar]
- 38.Minami K, Ogata J, Horishita T, et al. Intramuscular tramadol increases gastric pH during anesthesia. Can J Anaesth 2004;51:545–548. [DOI] [PubMed] [Google Scholar]
- 39.Beakley BD, Kaye AM, Kaye AD. Tramadol, pharmacology, side effects, and serotonin syndrome: a review. Pain Physician 2015;18:395–400. [PubMed] [Google Scholar]
- 40.Maréchal C, Honorat R, Claudet I. Serotonin syndrome induced by tramadol intoxication in an 8-month-old infant. Pediatr Neurol 2011;44:72–74. [DOI] [PubMed] [Google Scholar]
- 41.Rehni AK, Singh I, Kumar M. Tramadol-induced seizurogenic effect: a possible role of opioid-dependent γ-aminobutyric acid inhibitory pathway. Basic Clin Pharmacol Toxicol 2008;103:262–266. [DOI] [PubMed] [Google Scholar]
- 42.Rehni AK, Singh TG, Singh N, et al. Tramadol-induced seizurogenic effect: a possible role of opioid-dependent histamine (H1) receptor activation-linked mechanism. Naunyn Schmiedebergs Arch Pharmacol 2010;381:11–19. [DOI] [PubMed] [Google Scholar]
- 43.Claahsen-van der Grinten HL, Verbruggen I, et al. Different pharmacokinetics of tramadol in mothers treated for labour pain and in their neonates. Eur J Clin Pharmacol 2005;61:523–529. [DOI] [PubMed] [Google Scholar]
- 44.Product Information. Ultram. Ortho-McNeil-Janssen Pharmaceuticals, 2009.
- 45.Bloor M, Paech MJ, Kaye R. Tramadol in pregnancy and lactation. Int J Obstet Anesth 2012;21:163–167. [DOI] [PubMed] [Google Scholar]
- 46.Begg EJ. Prescribing in pregnancy and lactation. Br J Clin Pharmacol 2008;65:627–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhou SF. Polymorphism of human cytochrome P450 2D6 and its clinical significance. Clin Pharmacokinet 2009;48:761–804. [DOI] [PubMed] [Google Scholar]
- 48.Freye E, Levy J. Acute abstinence syndrome following abrupt cessation of long-term use of tramadol (Ultram): a case study. Eur J Pain 2000;4:307–311. [DOI] [PubMed] [Google Scholar]
- 49.Cicero TJ, Adams EH, Geller A. A postmarketing surveillance program to monitor Ultram (tramadol hydrochloride) abuse in the United States. Drug Alcohol Depend 1999;57:7–22. [DOI] [PubMed] [Google Scholar]
- 50.Senay EC, Adams EH, Geller A, et al. Physical dependence on Ultram (tramadol hydrochloride): both opioid-like and atypical withdrawal symptoms occur. Drug Alcohol Depend 2003;69:233–241. [DOI] [PubMed] [Google Scholar]
- 51.Willaschek C, Wolter E, Buchhorn R. Tramadol withdrawal in a neonate: how should it be treated? Eur J Clin Pharmacol 2009;65:645. [DOI] [PubMed] [Google Scholar]
- 52.Meyer FP, Rimasch H, Blaha B, et al. Tramadol withdrawal in a neonate. Eur J Clin Pharmacol 1997;53:159–160. [DOI] [PubMed] [Google Scholar]
- 53.Vazzana M, Andreani T, Fangueiro J, et al. Tramadol hydrochloride: pharmacokinetics, pharmacodynamics, adverse side effects, co-administration of drugs and new drug delivery systems. Biomed Pharmacother 2015;70:234–238. [DOI] [PubMed] [Google Scholar]
- 54.Tashakori A, Afshari R. Tramadol overdose as a cause of serotonin syndrome: a case series. Clin Toxicol (Phila) 2010;48:337–341. [DOI] [PubMed] [Google Scholar]
- 55.Tanne C, Javouhey E, Millet A, et al. Severe tramadol overdoses in children: a case series admitted to paediatric intensive care unit. J Clin Toxicol 2016;6:1–4. [Google Scholar]
- 56.Jovanović-Čupić V, Martinović Ž, Nešić N. Seizures associated with intoxication and abuse of tramadol. Clin Toxicol 2006;44:143–146. [DOI] [PubMed] [Google Scholar]
- 57.Talaie H, Panahandeh R, Fayaznouri MR, et al. Dose-independent occurrence of seizure with tramadol. J Med Toxicol 2009;5:63–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Oliva P, Aurilo C, Massimo F, et al. The antinociceptive effect of tramadol in the formalin test is mediated by the serotonergic component. Eur J Pharmacol 2002;445:179–185. [DOI] [PubMed] [Google Scholar]
- 59.Boostani R, Derakhshan S. Tramadol induced seizure: a 3-year study. Caspian J Intern Med 2012;3:484. [PMC free article] [PubMed] [Google Scholar]
- 60.Nelson EM, Philbrick AM. Avoiding serotonin syndrome: the nature of the interaction between tramadol and selective serotonin reuptake inhibitors. Ann Pharmacother 2012;46:1712–1716. [DOI] [PubMed] [Google Scholar]
- 61.Park SH, Wackernah RC, Stimmel GL. Serotonin syndrome: is it a reason to avoid the use of tramadol with antidepressants? J Pharm Pract 2014;27:71–78. [DOI] [PubMed] [Google Scholar]
- 62.Frank C. Recognition and treatment of serotonin syndrome. Can Fam Physician 2008;54:988–992. [PMC free article] [PubMed] [Google Scholar]
- 63.Safdari MR, Tavakoli M, Tafaghodi P, et al. Bilateral anterior shoulder dislocation following tramadol use. J North Khorasan Uni Med Sci 2015;7:939–945. [Google Scholar]
- 64.Rethnam U, Ulfin S, Sinha A. Post seizure anterior dislocation of shoulder – beware of recurrence. Seizure 2006;15:348–349. [DOI] [PubMed] [Google Scholar]
- 65.Betz ME, Traub SJ. Bilateral posterior shoulder dislocations following seizure. Intern Emerg Med 2007;2:63–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tantry TP, Kadam D, Shetty P, et al. Tramadol-induced respiratory depression in a morbidly obese patient with normal renal function. Indian J Anaesth 2011;55:318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Michaud K, Augsburger M, Romain N, et al. Fatal overdose of tramadol and alprazolam. Forensic Sci Int 1999;105:185–189. [DOI] [PubMed] [Google Scholar]
- 68.Nieuwenhuijs D, Bruce J, Drummond GB, et al. Influence of oral tramadol on the dynamic ventilatory response to carbon dioxide in healthy volunteers. Br J Anaesth 2001;87:860–865. [DOI] [PubMed] [Google Scholar]
- 69.Spiller HA, Gorman SE, Villalobos D, et al. Prospective multicenter evaluation of tramadol exposure. J Toxicol Clin Toxicol 1997;35:361–364. [DOI] [PubMed] [Google Scholar]
- 70.Hassanian-Moghaddam H, Rashidi B. Mortality and complication associated with acute tramadol intoxication. In: Clinical Toxicology 2008; 46:362–362.
- 71.Dayer P, Desmeules J, Collart L. The pharmacology of tramadol. Drugs 1997;53:18–24. [DOI] [PubMed] [Google Scholar]
- 72.Shadnia S, Soltaninejad K, Heydari K, et al. Tramadol intoxication: a review of 114 cases. Hum Exp Toxicol 2008;27:201–205. [DOI] [PubMed] [Google Scholar]
- 73.Lionte C, Bologa C, Sorodoc L. Toxic and Drug-induced Changes of the Electrocardiogram. INTECH Open Access Publisher; 2012. [Google Scholar]
- 74.Belin N, Clairet AL, Chocron S, et al. Refractory cardiogenic shock during tramadol poisoning: a case report. Cardiovasc Toxicol 2017;17:219–222. [DOI] [PubMed] [Google Scholar]
- 75.Memon S, Chhabra L, Masrur S, et al. Allergic acute coronary syndrome (Kounis syndrome). Proc (Bayl Univ Med Cent) 2015;28:358–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gormel S, Ege T, Koklu M, et al. Acute lateral myocardial infarction secondary to tramadol-induced Kounis syndrome. J Cardiothorac Vasc Anesth 2015;29:1599–1602. [DOI] [PubMed] [Google Scholar]
- 77.Keller GA, Etchegoyen MC, Fernandez N, et al. Tramadol induced QTc-interval prolongation: prevalence, clinical factors and correlation to plasma concentrations. Curr Drug Saf 2016;11:206–214. [DOI] [PubMed] [Google Scholar]
- 78.Clarot F, Goulle JP, Vaz E, et al. Fatal overdoses of tramadol: is benzodiazepine a risk factor of lethality? Forensic Sci Int 2003;134:57–61. [DOI] [PubMed] [Google Scholar]
- 79.Rahimi HR, Soltaninejad K, Shadnia S. Acute tramadol poisoning and its clinical and laboratory findings. J Res Med Sci 2014;19:855. [PMC free article] [PubMed] [Google Scholar]
- 80.Marquardt KA, Alsop JA, Albertson TE. Tramadol exposures reported to statewide poison control system. Ann Pharmacother 2005;39:1039–1044. [DOI] [PubMed] [Google Scholar]
- 81.Cao D, Heard K, Foran M, et al. Intravenous lipid emulsion in the emergency department: a systematic review of recent literature. J Emerg Med 2015;48:387–397. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors are responsible for data. Access to all relevant raw data will be free to any scientist.


